“The health of the child is the power of the nation.” — U.S. Children’s Bureau, 1918
“The health of the child is the power of the nation.” — U.S. Children’s Bureau, 1918
By large margins, the United States Senate and House of Representatives passed H.R. 2, the Medicare Access and CHIP Reauthorization Act of 2015, which was signed into law by President Obama on April 16, 2015. The centerpiece of the bill was a permanent repeal of the sustainable growth rate (SGR) formula that establishes Medicare payment rates for doctors. Although the legislation’s title implies equal billing for the Children’s Health Insurance Program (CHIP) and its “reauthorization”, the bill actually provides for just a two-year extension of funding — not a reauthorization of the program — that amounts to 2.7 percent of the bill’s overall spending.
 On the positive side, passage of the extension provides certainty that health coverage will continue for the more than 8 million children that rely on CHIP. Without question, that is immensely better than no extension of CHIP at all, as millions of children would have either lost coverage altogether or would have found alternative coverage to be significantly worse. In fact, the Urban Institute estimates that the number of uninsured children would have increased by 40 percent if CHIP were to have expired.
On the positive side, passage of the extension provides certainty that health coverage will continue for the more than 8 million children that rely on CHIP. Without question, that is immensely better than no extension of CHIP at all, as millions of children would have either lost coverage altogether or would have found alternative coverage to be significantly worse. In fact, the Urban Institute estimates that the number of uninsured children would have increased by 40 percent if CHIP were to have expired.
In addition, H.R. 2 provided two years of additional funding for several other important programs for children, including the Maternal, Infant and Early Childhood Home Visiting (MIECHV) program, Community Health Centers (CHCs), and Family-to-Family Health Information Centers (F2Fs) — all at current funding levels.
The inclusion of these provisions was definition very good news and, at both First Focus and the Campaign for Children, we are proud of our work toward these extensions. For example, the two organizations worked together or individually to:
- Organize a sign-on letter that garnered over 1,500 organizations in support of a four-year extension of CHIP;
- Organize a sign-on letter with over 750 organizations and individuals in support of the MIECHV extension;
- Meet with hundreds of congressional offices to educate them about the importance of CHIP and MIECHV to millions of children across this country;
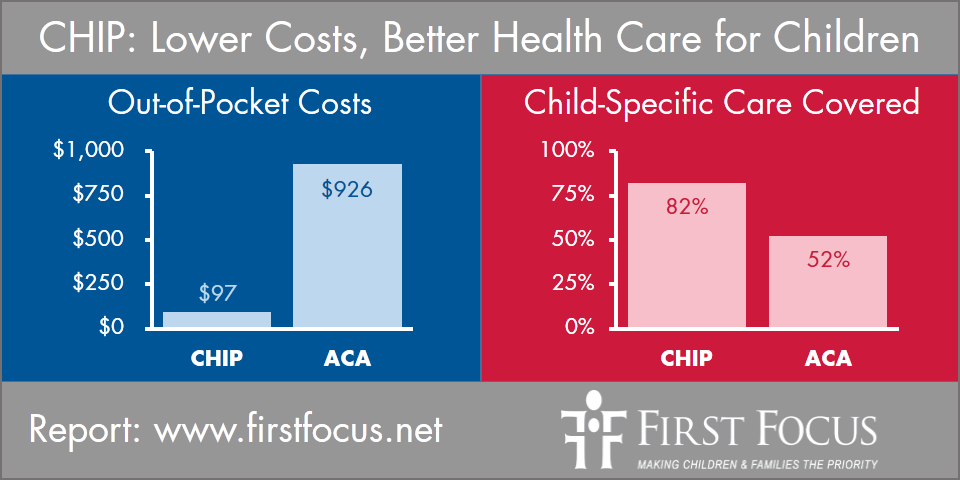
- Work closely with Wakely Consulting Group and disseminated their findings that found CHIP provides better benefits at significantly less cost to low-income families than coverage offered through the Affordable Care Act (ACA) exchange plans; and,
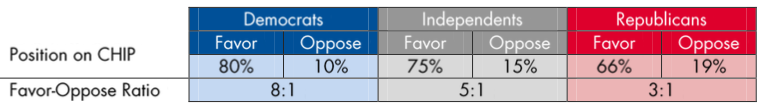
- Commissioned American Viewpoint, a Republican public opinion firm, to conduct a poll that found American voters supported the extension of CHIP by a 74–14 percent margin.
We thank all of those people that responded to our requests to sign-on to the letters and our emails or social media requests to contact Members of Congress in support of CHIP and MIECHV. We are also proud to have worked with outstanding coalitions of federal, state and local stakeholders in support of both CHIP and MIECHV.
However, due to the short timeframe of the extensions, any celebration must be short, as work must begin shortly to ensure that these programs are reauthorized in full in 2017.
The fact is that CHIP, MIECHV, CHCs, and F2Fs are all proven and effective programs that successfully have served our nation’s children well and deserve to be made permanent, just as H.R. 2 permanently extended the qualifying individual (QI) program and the transitional medical assistance (TMA) program in Medicare and Medicaid. Consequently, while we are certainly relieved that CHIP has been extended, we are less than jubilant that programs of important to children may have just been “SGR’d” or set up to be continuously included in short-term, health care “extenders” bills.
The untold story is that both Democrats and Republicans in Congress supported a four-year extension of CHIP, as was called for by over 1,500 federal, state, and local organizations across the country.
The fact is that CHIP works…and works very well for children.
As for MIECHV, Jonathan Cohn of the Huffington Post points out that, like CHIP, the program has bipartisan support because of its strong evidence-based background. As he writes in his article entitled “This May Be The Most Effective Anti-Poverty Program in America”:
“…if home visiting is successful on a large scale, it could prove transformative. While paying trained nurses and social workers to visit homes can get expensive, at least in the beginning, it can also yield large returns later on — in the form of a more productive workforce, as well as taxpayer dollars not spent on treatment for mental and physical health problems, public assistance and the criminal justice system.”
Rep. Charles Boustany (R-LA) adds:
“This bill addresses an issue that isn’t addressed enough in Congress — the importance of using evidence to figure out what works to reduce poverty in America. This program is designed to improve outcomes for children and families — especially those children who face the greatest risk of abuse and neglect.”
But, to do a full evaluation of MIECHV and to allow states to make investments to continue to improve the quality of both programs and to look at longer-term trends in their effectiveness, grants to states need to be longer than for just two years.
With respect to CHIP, the time-period for the extension was actually caught up in a dispute over the matching rate that the federal government would give to states in CHIP in FY 2016 and beyond.
The current average federal/state matching rate for CHIP is 71/29 but, under the ACA, a provision was added by Senator Jay Rockefeller (D-WV) to increase the federal matching rate for CHIP by another 23 percentage points beginning in FY 2016. This provision, known as the “CHIP bump,” would raise the federal matching rate to an average federal share of over 90 percent next year and, thereby, increase federal spending and lower state spending in CHIP by billions of dollars a year. In fact, the CHIP bump raises the federal match to 100 percent in 11 states and over 95 percent in 24 states and the District of Columbia.
The winners here are the states, as billions of dollars in additional federal money flows to them while their corresponding state matching rate contribution to CHIP declines dramatically. For example, the State of North Carolina will see its state share of CHIP decline from 23.9 percent in 2015 to just 0.4 percent in 2016.
Some ACA proponents, including a number of congressional Democrats, argued that the federal funding windfall to states, which will cost the federal government an estimated $7 billion in increased federal spending in CHIP over two years, was important to incentivize states to take up the ACA’s Medicaid expansion option to expand coverage to adults — not children.
In contrast, Senator Orrin Hatch (R-UT) and Representative (R-MI) argued in their CHIP extension discussion draft that:
“Democrats and Republicans in Congress — and governors of both parties — have hailed [CHIP] as a success at the current match rate. [The Congressional Budget Office] also estimates that no new net enrollment will result from maintaining the 23 percent funding increase. Therefore, there is no policy justification to continue to direct federal taxpayer dollars to efforts that do not impact coverage for low-income children.”
It is important to note that an extension of CHIP would have actually saved federal funding in Congress had not included the 23 percentage point increase in the federal matching rate.
Instead, $6–7 billion was spent in H.R. 2 over two years to purposely give states a fiscal windfall through a pretty significant increase the federal match in CHIP. Fortunately, a number of child advocates are working in the states, with varying degrees of success, to push for states to ensure that money remains dedicated to children. However, child advocates can only wonder what important changes to child well-being could have been achieved if those billions of dollars had been dedicated directly to children instead of to states.
Moreover, as advocates for CHIP, we are deeply concerned that increasing the federal cost of CHIP makes subsequent extensions of the program more difficult and potentially leads to waste in the program, as states with close to or the full 100 percent federal matching rate will have little incentive to control health care or administrative costs.
The concern is that funding that should be dedicated to the health of millions of children could be diverted to waste, fraud, or abuse. Furthermore, for those states with no match requirement in CHIP and that have provider taxes, they will actually “make money” on CHIP payments to providers.
On the other hand, it is not correct to say there is “no policy justification” for some increase in the federal matching rate in CHIP. If Congress had completely eliminated the “CHIP bump,” coverage for children in Medicaid will have an average federal matching rate of 57 percent and children’s coverage in CHIP would have been left at an average of 71 percent.
The problem here is that the health costs to adults below 138 percent of the poverty line in Medicaid currently have a 100 percent federal matching rate that is scheduled to decline to 90 percent by FY 2020. By having the matching rate for children’s coverage at a significantly lower rate than for adults, this creates a negative incentive for states to look to cut, restrict, or disadvantage pediatric payments and children’s coverage if the state were to face shortfalls or tight state budgets in the future.
For child advocates, with both parties supporting an extension of CHIP for four years, the hope was for the two political parties to have reached a compromise on the federal-state matching rate extremes. For example, Congress could have limited the maximum CHIP matching rate to 90 percent and possibly changed the CHIP administrative match to be the same as Medicaid’s. These alternative matching rates would still address Senator Rockefeller’s worthy goal of eliminating the disparate matching rates between children in CHIP and adults in the ACA will lowering federal CHIP spending because states would:
- Have “skin the game” in order to run a more efficient program;
- Better ensure funding dedicated to children are appropriately spent to improve child health and not on administrative costs and waste; and,
- No longer have the option of “making money” on CHIP expenditures through the receipt of provider taxes and donations and intergovernmental transfers.
Unfortunately, rather than finding a compromise in the best interest of children, the fight on CHIP was focused on the politics around the ACA. Although congressional Republicans gave into the demand to leave the ACA’s 23 percentage point increase intact, they countered that they could then only agree to a two-year extension of this ACA provision. Consequently, the final language in H.R. 2 left in place the CHIP bump but cut the extension of the program back to just two years.
Revisiting the matching rate issues will, undoubtedly, be necessary to extend CHIP in 2017. However, efforts to address the possible problems associated with having 100 percent federal match in CHIP will likely be met with opposition from some states and ACA proponents.
CHIP advocates will also face a number of other important barriers to extending the program in 2017. The second major challenge is associated with the fact that the House of Representatives actually did not even fully fund the two-year extension of CHIP. To reach an arbitrary spending level of $5.6 billion over two years, the House created a budget gimmick and “clawback” that raids one-third of all carryover funding in FY 2018 (see Section 301 in H.R. 2) from unspent FY 2017 state allotments and, instead, has those dollars that had been dedicated to children’s health revert to the Federal Treasury.
Although this arbitrarily lowers the CBO score for CHIP in the short-term, the clawback creates a bigger funding hole in FY 2018 that Congress will have to fill in a 2017 reauthorization of the program.
CHIP has also always had a funding cliff where Congress arbitrarily sets the out-year spending levels arbitrarily low in order to meet out-year budget targets. Unfortunately, although the Hatch-Upton discussion draft suggested the option of eliminating CHIP’s funding cliff, H.R. 2 not only extended the cliff but added the FY 2018 clawback. As a result, Congress will now have to address both the funding cliff and clawback.
Third, because CHIP is popular, there will be some that may attempt to hijack or take CHIP’s reauthorization hostage in order to pursue other political agendas in 2017. Grace-Marie Turner with the Galen Institute previewed one possible attempt in a recent Forbes article where she spoke in favor of passage of H.R. 2 and added:
“In addition, the deal would extend the Children’s Health Insurance Program (CHIP) for two years. It is due to expire September 30, and the extension buys time for a new president to tackle health reform and begin to streamline the government’s wastefully-siloed health spending programs, including Medicaid, CHIP, and ObamaCare.”
Fourth, CHIP may now bear enormous weight as the vehicle for other health programs that will need to be extended. As Erin Mershon with POLITICO writes:
“Even as lawmakers celebrate the demise of the SGR, their success on that issue may have shifted pressure onto a different one: the Children’s Health Insurance Program.
The permanent repeal of the flawed Medicare payment formula means Congress has one less legislative vehicle on which to load provisions extending, ending or reauthorizing other health-related programs — from Medicare therapy caps to continued funding for rural hospitals to CHIP itself. Lawmakers’ short-term patches for the Sustainable Growth Rate sometimes included dozens of such add-ons.”
While others may be glad that CHIP will be around in 2017 to potentially lead the extenders package, First Focus’s Ed Walz points out that is problematic for CHIP. As he points out:
“That’s a big concern, because ‘extender vehicle’ translates pretty consistently into ‘done-at-the-last-minute.’ As dozens of governors told Congress last year, last-minute action on CHIP doesn’t work for states — or for kids.”
Cathy Caldwell, Alabama’s All KIDS CHIP program director, adds:
“The bottom line is that two years is better than no continuation of funding, but. . .it still leaves us in a state of uncertainty. I don’t think two years is long enough to fix the things that need to go in place for children to go into marketplace insurance plans.”
Consequently, as advocates celebrate the two-year extensions that Congress granted to programs of importance to children, there are a number of challenges facing both CHIP and MIECHV in 2017 that must be addressed. We should begin today to figure out what is the best solution for the future of children as soon as possible.
For example, MIECHV will need to be fully reauthorized in 2017.
And in the case of CHIP, there are a number of questions that arise. For example, should we fully reauthorize CHIP, as it remains clearly superior to any alternative coverage for children? Should we fold CHIP into the ACA exchange plans after fixing some significant shortcoming in the ACA exchange plans (e.g., the “family glitch,” benefits, cost sharing, and provider networks) so that children could receive at least comparable coverage? Or, is there some other alternative that should be considered, such as the use of section 1322 state waivers included in the ACA for children?
There is much to consider and that is why child advocates, in particular, must get into “the game” as soon as possible because the decision over which option is chosen must be made based on what is in the best interest of our nation’s children.
This blog post was originally published in Medium.
The Health of the Child is the Power of the Nation: http://bit.ly/1EiXMQ5 v/ @First_Focus #CHIPworks #HomeVisiting pic.twitter.com/JN1o0RoixH
![]() Tweet this now.
Tweet this now.
Tweet the author: @BruceLesley
Want to learn more? First Focus is a bipartisan advocacy organization dedicated to making children and families the priority in federal policy and budget decisions. Learn more about our work on child health.
Want to get involved? You can support our work on child health by making a donation or joining our mailing list to receive updates and action alerts on this issue.